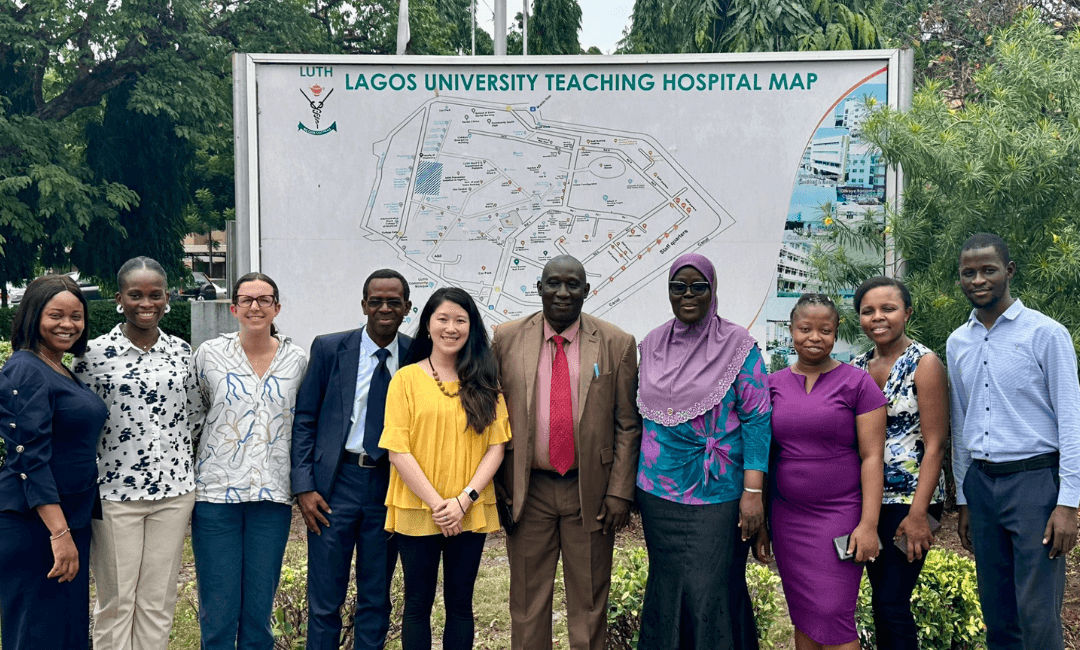
Dr. Julia Xu with collaborators at Lagos University, Nigeria. photo source
Sickle cell disease affects more than 100,000 people in the United States, where it is considered a rare disease. But in sub-Saharan Africa, it is far more common and a major contributor to childhood mortality. The region carries the highest global burden, with most children born with the disease dying before the age of five due to lack of early diagnosis and treatment. Researchers in the Department of Medicine’s Division of Classical Hematology and the Vascular Medicine Institute are leading efforts to combat the effects of sickle cell disease across Africa through a series of collaborative clinical trials and studies. In partnership with local institutions in countries including Ghana and Nigeria, Drs. Enrico Novelli, Busola Oluwole, and Julia Xu are working to improve early detection and treatment by screening newborns, testing new approaches to manage pain in pregnant women, and exploring how existing drugs can be repurposed to treat anemia.
Reducing Under-Five Mortality (U5M) in Sub-Saharan Africa
Sickle cell disease can begin causing serious complications as early as six months of age, once the protective effects of fetal hemoglobin wear off. One of the most dangerous complications is sepsis, life-threatening infections that occur because children with sickle cell often lose spleen function very early. In many countries, a simple blood test at birth allows for early diagnosis, and with prompt treatment, including penicillin and routine vaccinations, sepsis-related deaths can largely be prevented. However, in sub-Saharan Africa, where newborn screening is not yet widespread, sickle cell disease remains a leading cause of death in children under five.
Dr. Enrico Novelli serves as co-chair of the Consortium on Newborn Screening in Africa (CONSA), an initiative working to establish training programs, implement newborn screening, and evaluate the effectiveness of early interventions across seven sub-Saharan countries: Ghana, Kenya, Liberia, Nigeria, Tanzania, Uganda, and Zambia. Children are screened and treated according to a shared protocol, and their outcomes are tracked through a centralized database. The goal is to demonstrate that early detection and treatment can significantly reduce under-five mortality, and to use this evidence to advocate for national adoption of newborn screening programs beyond the pilot sites.
Identifying sickle cell disease early is just the first step. Improving quality of life across the lifespan is equally important. One area where better support is urgently needed is in managing pain, particularly for pregnant women who face limited treatment options.
Mitigating Pain During Pregnancy in Ghana
When pregnant women with sickle cell disease experience acute pain episodes, many standard pain medications and disease-modifying treatments are off-limits due to potential risks to the baby, leaving a critical gap in care. To help these patients safely find relief, Dr. Busola Oluwole is launching a feasibility trial in Ghana to explore whether digital cognitive behavioral therapy (CBT) can offer a safe and effective alternative for managing pain during pregnancy. These episodes are often intensified by stress, anxiety, and depression—factors that can be especially heightened during pregnancy—making CBT a promising, non-pharmacologic approach.
The study will use a mobile app, offering patients a 12-week CBT program supported by a health coach to reinforce learned skills. Previous research in Ghana has shown that pain during pregnancy often escalates in the third trimester and is frequently self-managed at home. By providing accessible, structured support through the app, this intervention may help women better manage—and potentially prevent—these painful episodes.
Beyond pain, chronic anemia remains one of the most debilitating aspects of sickle cell disease, contributing to organ damage and poor physical function. Pitt researchers are also working to address this challenge through innovative clinical trials in both Nigeria and the U.S.
Advancing Anemia Treatment in Nigeria
Dr. Julia Xu, in collaboration with researchers at Lagos University Teaching Hospital, recently completed a pilot clinical trial aimed at addressing anemia in patients with sickle cell disease in Nigeria. Anemia is a major driver of organ damage and reduced quality of life in these patients, yet treatment options are extremely limited. The only approved drug specifically targeting anemia in sickle cell disease, voxelotor (Oxbryta), was withdrawn from the market in 2024, leaving clinicians with no approved alternatives.
To explore a new approach, Dr. Xu’s team tested the addition of erythropoietin (EPO)—a drug that stimulates red blood cell production—to the standard treatment regimen of hydroxyurea. In collaboration with Dr. Titilope Adeyemo at Lagos University Teaching Hospital in Nigeria, the team enrolled patients in both Lagos and Pittsburgh. While the full results are still in progress, preliminary findings are highly encouraging, with participants showing significant increases in hemoglobin levels, improved performance on the six-minute walk test (a measure of physical function), and favorable changes in blood biomarkers such as reduced red cell breakdown.
Despite these promising outcomes, access to EPO remains a major barrier. In Nigeria, where health insurance coverage is minimal, patients must pay out of pocket for EPO, which is prohibitively expensive. Similar access issues exist in the U.S., where EPO is often not covered by insurance for sickle cell patients, limiting its availability even in high-resource settings.
To support and strengthen future multinational trials, Dr. Xu is partnering with Functional Fluidics, a biotech startup company founded by Dr. Patrick Hines, which has established a commercial lab in Nigeria specializing in advanced red blood cell function testing. The collaboration aims to compare red blood cell characteristics, such as deformability and adhesion, in sickle cell patients in Nigeria and the U.S. Understanding biological differences between these populations is essential for interpreting clinical trial results, optimizing treatment responses across diverse groups, and helping to inform effective global strategies for treating sickle cell anemia.
Taken together, these initiatives reflect a bold, collaborative approach to changing the outlook for sickle cell disease—not only in Africa, but globally. By focusing on early diagnosis, improving care for vulnerable populations, finding cost-effective treatments, and optimizing use of existing medications, researchers are helping to change the trajectory of sickle cell disease in some of the hardest-hit regions. As studies continue, the knowledge gained and partnerships built will not only benefit communities in Africa, but also shape the future of sickle cell care worldwide.
If you’d like to support our work, these funds represent the programs in most need of philanthropic support:
The Sickle Cell Disease Fund was created to support various projects involving sickle cell disease, such as Research Day and Advocacy Day for Sickle Cell Patients, outreach education for sickle cell disease patients and determining ways to engage patients who do not routinely attend support groups due to illness.
All donations to the division are important and welcomed. Unrestricted donations to the General Fund are especially essential because they provide the greatest flexibility of use. Your gift might be used for a current research study, to fund novel paths of discovery, to support the training of future hematology specialists or for continuing professional development of clinical staff.
Gifts to this fund enable the Vascular Medicine Institute to perform rigorous, cutting-edge basic and translational research in vascular biology. Training the next generation of scientists in bench-to-bedside translational research is crucial to this mission.